As humans, we use language to shape how we perceive the world and the people around us. We have a choice of words to describe ourselves and others. Our choice of words influences how we view mental health and well-being. Considering the impact of language on people’s thoughts and beliefs, it is imperative to carefully use language with individuals suffering from mental health conditions to positively influence their healthcare treatment.
Linguists say that words carry a wide array of positive and negative connotations attached to them. It could be assumed that different people might have different associations or connotations of words. The same applies to mental health treatment, where individuals might not prefer specific stigmatised words to be used. In the context of mental illness, mental health, and well-being, negative words can be experienced as condescending, isolating, and stigmatising, while positive words can convey dignity, empathy, and hope (1).
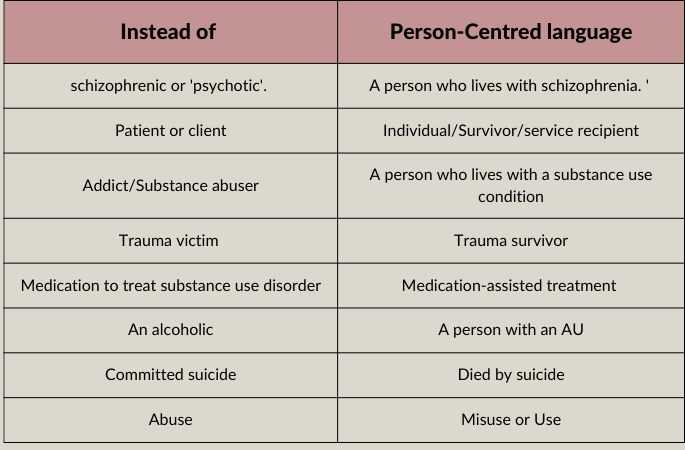
A growing body of literature provides comprehensive guidelines for communicating about mental health conditions in a non-stigmatising manner. Researchers and institutions must engage directly with people with mental illnesses to understand what they prefer when it comes to non-stigmatising language. Despite the fact that language norms constantly evolve, not all groups of patients agree on preferred terms. Researchers, clinicians and other individuals who deal with or communicate about mental disorders emphasise the importance of using neutral, person-centred language rather than potentially stigmatising words and labels. The person-centred language implies that a person’s illness or disorder is only one aspect of their life, not their defining characteristic (2). Utilising person-centred language is critical to ensure the recovery of people with mental health disorders. Therefore, language should be evaluated in terms of how it reinforces negative biases or encourages empowerment (1). Below are some examples of person-centred language (2, 3).
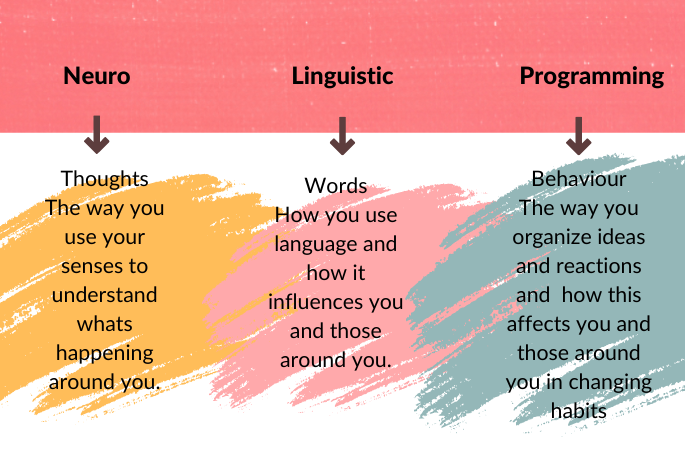
Neurolinguistics programming (NLP) is another approach that can help healthcare providers understand the unconscious minds of people with mental illnesses and change their patterns of mental and emotional behaviour. It is a model of human behaviour and cognition that describes how people represent their world by interacting and communicating with one another, how they experience distress and disappointment, and how it helps change their representation of the world to relieve their distress and cope with life more effectively, with more fulfilment (4). Also, the NLP model supports the use of the preferred language when interacting with others, so people with mental illnesses may also benefit from its application.
 We construct our thoughts and inner realities using language; we adjust our language patterns to align with those around us and build rapport through the similarity of our language patterns. One of the tenets of NLP is Rapport-building; it is the heart of Neurolinguistic Programming (NLP), leading to successful communication between individuals or groups. In the context of mental well-being, it can give a healthcare provider a great deal of power to connect with people with mental conditions. As they begin to understand their world, they may develop a deeper understanding of their world and the problems they have been facing in their lives (5, 6). Neurolinguistic programming (NLP) therapies have also been used for specific behavioural outcomes, including the resolution of phobias, posttraumatic stress disorder flashbacks, internal conflicts, anxiety, grief, and many other problems and effects. Also, clinical and practitioner evidence is available that supports NLP therapies as a treatment for individuals having these behaviours (7).
We construct our thoughts and inner realities using language; we adjust our language patterns to align with those around us and build rapport through the similarity of our language patterns. One of the tenets of NLP is Rapport-building; it is the heart of Neurolinguistic Programming (NLP), leading to successful communication between individuals or groups. In the context of mental well-being, it can give a healthcare provider a great deal of power to connect with people with mental conditions. As they begin to understand their world, they may develop a deeper understanding of their world and the problems they have been facing in their lives (5, 6). Neurolinguistic programming (NLP) therapies have also been used for specific behavioural outcomes, including the resolution of phobias, posttraumatic stress disorder flashbacks, internal conflicts, anxiety, grief, and many other problems and effects. Also, clinical and practitioner evidence is available that supports NLP therapies as a treatment for individuals having these behaviours (7).
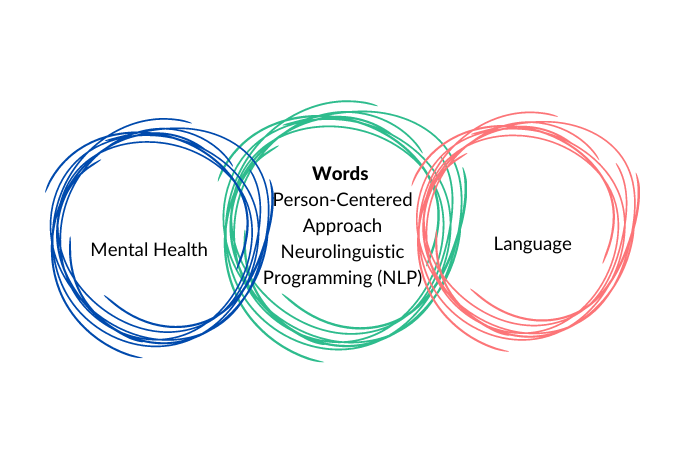
In summary, appropriate and non-stigmatised language can help promote a person-centred framing of the condition, which implicitly reinforces that individuals with mental health conditions deserve compassion and care. This shift in mindset is crucial to treating individuals suffering from mental health conditions. Therefore, it is asserted that counsellors, therapists, and communicators can enhance their effectiveness in helping individuals by incorporating a person-centred approach and NLP therapies, which in turn help to reduce stigma and promote appropriate, respectful and empowering language for their better well-being (1).
References
1. Richards V. The importance of language in mental health care. Lancet
Psychiatry. 2021.
2. Volkow ND, Gordon JA, Koob GF. Choosing appropriate language to reduce
the stigma around mental illness and substance use disorders.
Neuropsychopharmacology. 2021
3. health HFfm. Language Matters in Mental Health. In: 2022 HF, editor. Hogg
Foundation for mental health. 1st ed. 3001 Lake Austin Blvd, Austin, TX
787032022.
4. Heap M, Neurolinguistic programming: What is the evidence? In D. Waxman,
D. Pedersen, I. Wilkie & P. Mellett (Eds.) Hypnosis. Whurr Publishers. 1989.
5. Ready R, and Burton K. Neuro-linguistic Programming For Dummies. 2nd ed.
John Wiley & Sons, Ltd; 2010.
6. Hoobyar T, Dotz T, Sanders S. The Essential Guide To Neuro Linguistic
Programming From NLP Comprehensive. William Morrow; 2013.
7. Wake L, Gray R, Bourke F. The Clinical Effectiveness of Neurolinguistic
Programming
A Critical Appraisal. 1 st ed. Routledge; 2013.



